Recognising and Responding to Acute Deterioration Policy Review
Overview
The Recognising and Responding to Acute Deterioration Mandatory Policy MP 017/22 (RRAD policy) is a mandatory requirement under the WA Department of Health Clinical Governance, Safety and Quality Policy Framework.
The RRAD policy provides consistent clinical guidance to Health Service Providers (HSPs) by setting the minimum requirements to be implemented by HSPs through the development of local evidence-based policies and systems, to facilitate early recognition and response to acute deterioration in their setting.
This policy aligns with the National Safety and Quality Health Service (NSQHS) Standard 8: Recognising and Responding to Acute Deterioration, mandated in WA through the National Safety and Quality Health Service Standards Accreditation Policy - MP 0134/20.
The RRAD policy supports the use of clinician, patient, support people and carer’s judgement, in addition to mandatory elements, to escalate care.
Why your views matter
The RRAD policy is approaching the 3-year policy review requirement. The Patient Safety and Clinical Quality Directorate (PSCQ) has prepared a revised policy, informed by initial stakeholder consultation with Health Service Provider RRAD Committees and related units in the Department
The Department of Health (the Department) is seeking feedback from consumers, family members, support people and, clinical and non-clinical WA Health employees representing the Health Service Providers on the proposed policy amendments.
In 2023/24, WA Health system data showed there were 1,691 clinical incidents associated with acute deterioration. This Standard had the highest number of incidents resulting in patient deaths, based on notifiable data.
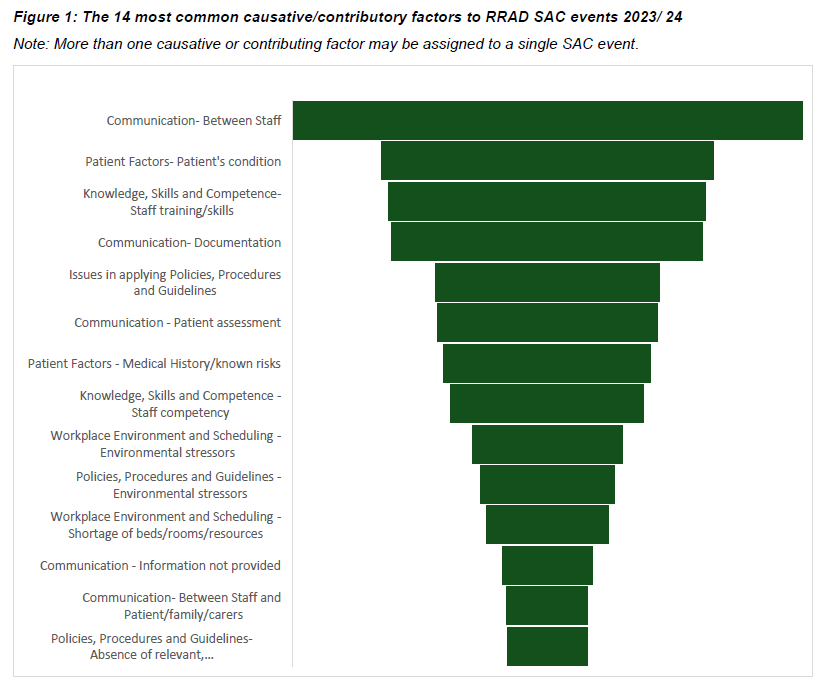
Communication between staff was identified as the major causative or contributory factor of the investigated acute deterioration clinical incidents. Knowledge, skills and competence, documentation, and issues in implementing policy, procedure or guidelines, were amongst the top 5 causative or contributory or causative factors (Figure 1).
Figure 1 shows the 14 most common factors contributing to acute deterioration, based on their frequency in 2023-24 of the most severe clinical incident (SAC1) investigations.
Audiences
- Aboriginal health
- Aboriginal Health
- Aboriginal Health
- Allied Health
- Allied Health
- Consumers
- Consumers
- Department of Health
- Department of Health Executive
- Doctors
- Doctors
- Doctors
- Health professionals
- Health Service Providers
- Health workforce
- Local governments
- Midwife
- Non-government organisations
- Nurses
- Nurses
- Planning
- Planning
- Planning
- Policy
- Policy
- Policy
- Population Health
- Primary Care Teams
- Public and Aboriginal Health Division
- Research institutions
- Researchers
- Royal St Staff
- State government agencies
- WA Health
- WA Health Service Providers
- WA Health services and staff
Interests
- Aged Care
- Alcohol and Other Drugs
- Cancer
- Cardiology
- Cardiovascular
- Child and Youth Health
- Child Health
- Clinical Excellence
- Consumer engagement
- Consumer/carer/community engagement
- Department of Health Executive
- Diabetes and Endocrine
- Digestive
- Disability
- Endocrinology
- Falls Prevention
- Feedback
- Genetics
- Infections and Immunology
- Infectious Diseases
- Injury and Trauma
- Lifestyle
- Mental Health
- Mental Health
- Mental Health
- Musculoskeletal
- Neurosciences and the Senses
- Opthalmology
- Oral Health
- Palliative Care
- Patient Safety and Clinical Quality
- Pharmacology
- Planning
- Policy development
- Policy development
- Primary Care
- Renal Health
- Respiratory
- Respiratory Health
- Strategic Policy
- Women's and Newborn's

Share
Share on Twitter Share on Facebook